Unspoken truths behind UC
Identifying the unspoken truths behind uncontrolled UC
Uncontrolled UC may have a negative impact on patients’ daily lives.

81%
of patients who self-reported being in remission indicated that UC affected their ability to go to work2,a,b
The majority
of patients who met predefined criteria for remissionc reported that UC impacted their social activities3,d
UC can impact many aspects of a patient’s life. The intimacy of UC and embarrassment patients sometimes feel around the condition can make it difficult for them to share the full impact of their disease when in consultation with their physician. Even when patients are comfortable sharing their experience of UC, some may simply forget how much they're limiting their life due to their condition because of settling behaviours. This can make it challenging for physicians to identify when their disease may no longer be controlled.
Can you identify the unspoken truths in these patient experiences?
Read the cards below, then flip them over to discover the unspoken truth, which, if shared, may have indicated that these patients have uncontrolled UC.

Amadou
31 years old, male patienta
Diagnosed 5 years ago with extensive colitis. Initially prescribed oral 5‑aminosalicylates (5-ASAs); corticosteroids (CSs) were added after a series of flares, became CS dependent; continued with oral 5-ASAs and azathioprine was added to wean off CSs; achieved clinical remission, but requested to be taken off azathioprine after ~3 years because, similar to when he was CS dependent, he experienced repeated infections; continued oral 5-ASAs; topical 5-ASAs were prescribed ~1 year ago to treat persistent symptoms; not currently prescribed CS.


“I’m a bit tired and stressed out, but otherwise good. Thanks for recommending the patient organisation. Their website helped me understand my treatment options and has convinced me that my current UC treatment is a good fit for me – reading about the side effects of some other drugs made my spine shiver thinking of the…
…infections I went through with the last treatment. I’m doing OK on my new meds. Soccer? No, I had to quit the team unfortunately, I’ve had a busy period at work, and I was finding it hard to keep up with the demands of both work and soccer.”
Amadou has not disclosed to his doctor that he is still experiencing abdominal pain on his current treatment. He is highly health literate and is aware this means he will likely require advanced therapy, but he has downplayed his symptoms because of his safety concerns. Given his previous history with infections, and extensive reading on the adverse events of existing advanced therapies, he feels a sense of dread at the prospect of starting an advanced therapy. Amadou is highly stressed because of his situation. The persistent symptoms are affecting his social life, causing him to quit the soccer team he was captain of, something he took great pride in.
What questions would you ask to better understand a patient's experience with UC?

Júlia
27 years old, female patienta
Diagnosed 2 years ago with left-sided colitis; clinical remission maintained on oral 5-ASAs.


My UC is fine, honestly. I don't really go to the toilet much more than normal. Maybe 2-4 times a day total? I try to keep it to less than that as I'm too busy with work. I love my job, and my media clients; we had 3 workshops with …
… them last week and we’re gearing up for a really intense period. So, of course I’m run down at the end of the day, but who isn’t? No one said having a chronic disease was easy! Of course, you have to make compromises.”
Recently, Júlia has had a recurrence of some symptoms (abdominal pain; diarrhoea), which have worried her that she may have to step away from client work – work she really values. To manage this, she has started skipping meals4 and avoiding certain foods and social situations involving food in an attempt to reduce her number of daily stools. This has led to fatigue and light-headedness during the working day.
Can you think of a patient like Júlia, whose resilience is impacting their quality of life?

Markus
39 years old, male patienta
Diagnosed 3 years ago with isolated proctitis; initial symptoms (stool frequency and rectal bleeding) were treated with topical 5-ASAs, oral 5‑ASAs were added after symptoms persisted; symptoms continued so topical and oral CSs were added.


A lot has happened since we last spoke. I’ve sadly left the band. I can’t keep up with the live shows these days. Instead, I’ve started music lessons from home. It’s definitely a step down from the stage but working from…
…home is a better fit for me these days. My UC is OK, I think. I’ve had no bleeding since we started the steroid foam. It would be nice to know a bit more about my type of UC – isolated proctitis, I think it’s called?”
Live music has become increasingly difficult for Markus. Having to apply the topical foam backstage before a gig was neither convenient nor a pleasant experience. What’s more, he started to experience troublesome symptoms more frequently. Markus is embarrassed to talk about it, but he has experienced accidents at work during gigs due to sudden onset of bowel urgency. This has negatively impacted his ability to work, because he always needs to know where the nearest toilet is. Despite his passion for live music, he felt he could only function fully within the comfort of his own home, so he quit the band and started teaching music from home instead.
Do you know any patients with UC who have shaped their life around their disease?
aFictional patient case.
Settling for “OK”
Why might patients with UC settle for “OK”?
Patients with UC may exhibit settling behaviours if they have low expectations of what it means to be in clinical remission.


Patients with UC do not always fully communicate what they wish to discuss during consultations with their physicians.

worried that if they asked too many questions then their physician would see them as a difficult patient, which would affect the quality of care they received6,a
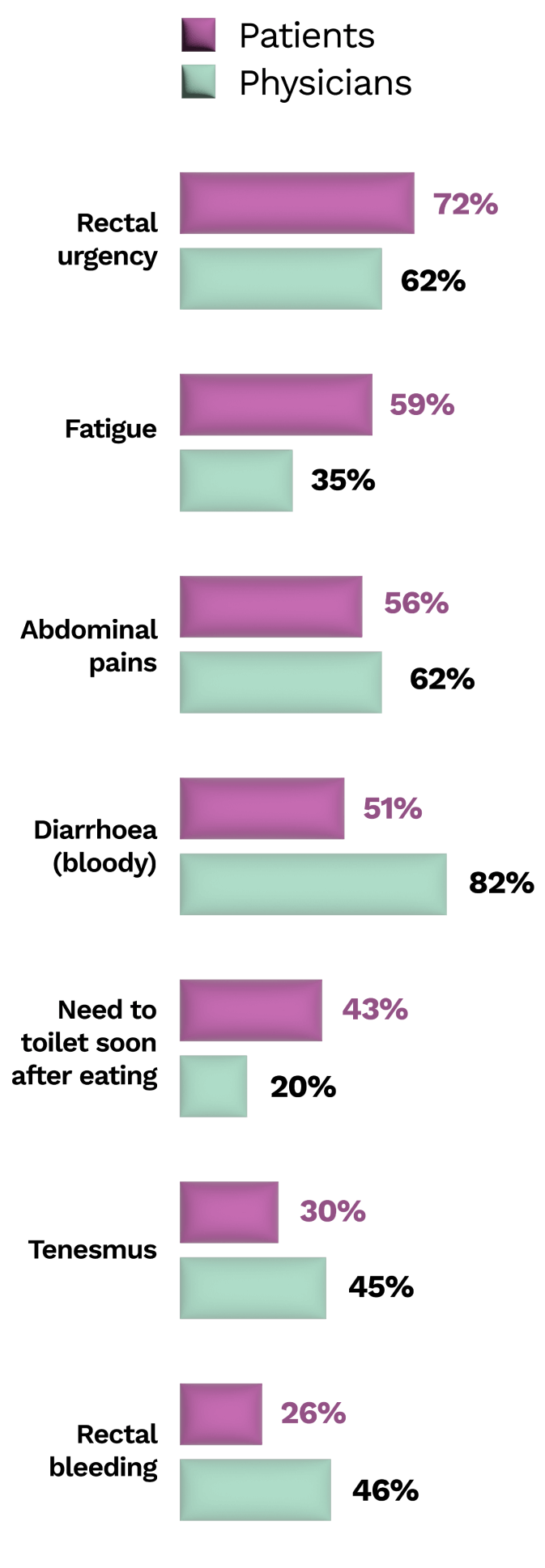
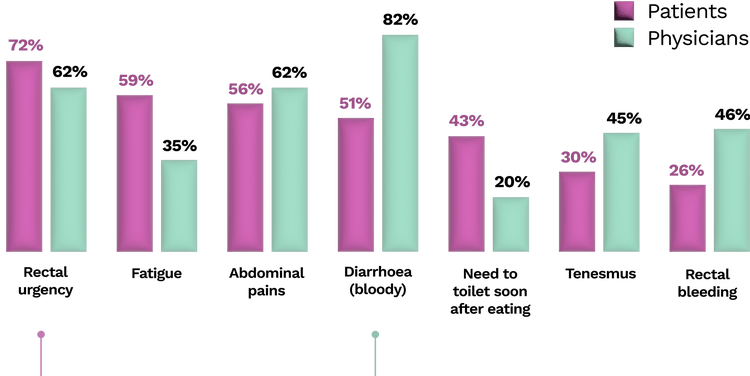
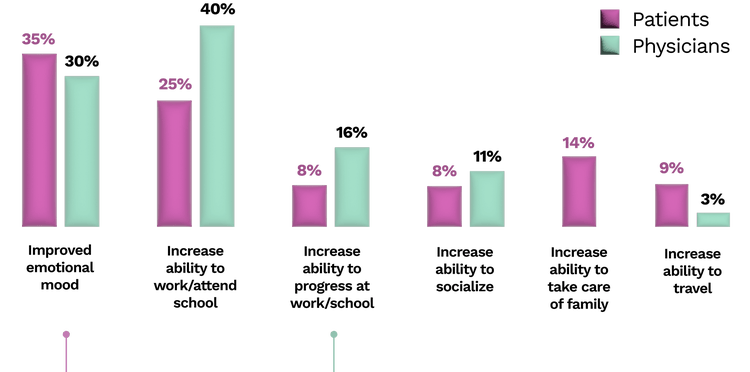
There is misalignment between patients and physicians on what UC symptoms have the greatest impact on quality of life.7
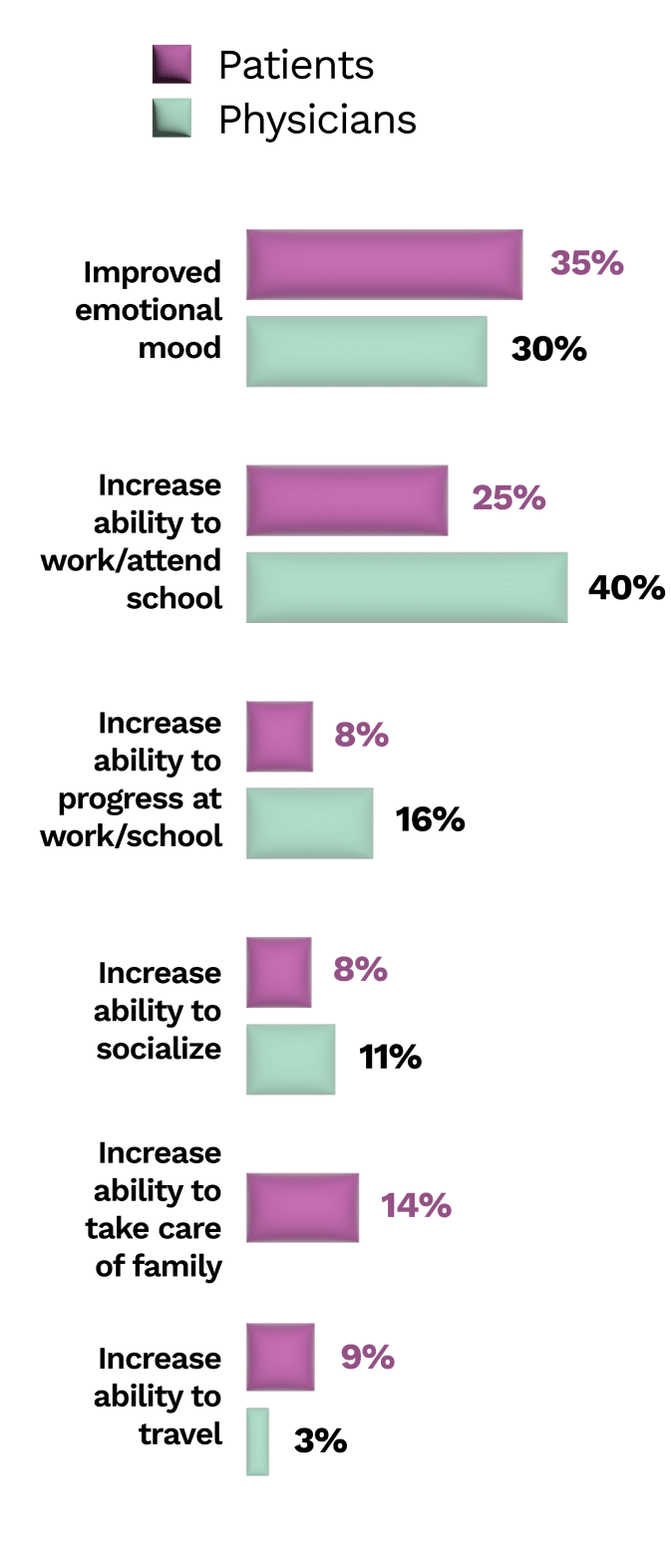
There is misalignment on treatment goals between patients with UC and their physicians.7

In a survey, 30% of patients with UC rated the impact of UC on their mental wellbeing as an aspect that they wished their physician had a better understanding of.2,a

However, only 23% of physicians reported regularly discussing this topic with their patients2,a
The prevalence and impact of uncontrolled UC
Patients with UC frequently experience ongoing symptoms on conventional therapies or lose response over time.5,8,9

of patients on conventional therapy reported ongoing symptoms of rectal bleeding5,a

of patients on 5-ASA maintenance therapy failed to maintain clinical or endoscopic remission at 6–12 months8,b

of patients with moderate to severely active UC had significant worsening of UC or onset of acute symptoms after initiating immunomodulating therapy (mean of ~5 months)9,c
Excessive use of and dependency on CSs in patients with UC is common and often avoidable.10
16.2%
of patients with UC in a multicentre audit met the definition of steroid dependency or excess,a of which approximately half of the cases were considered avoidable10,b

A substantial proportion of patients with IBD are not prescribed advanced therapies despite being appropriate for treatment according to study criteria.11
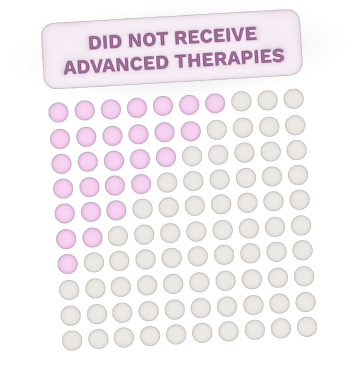
28.6%
of patients did not receive advanced therapies despite being appropriate for treatment according to study criteria1,a,b
There remains a need for additional therapeutic options in UC that are preferably oral,12 effective, and have minimal side effects.5
>90%
of patients with IBD rated tablets highly acceptable compared with granules, infusions, and subcutaneous injections.13,a
Resources to help look behind “OK” for patients’ UC
Recognising the true impact of UC on a patient's quality of life and timely identification of when their disease may be uncontrolled can be a challenge in regular practice, particularly if there is limited time with the patient.
Here are some practical resources to help you and your patients have deeper conversations to bridge this gap to help them get back to their baseline.
For you
Effective Dialogue RESOURCE
This resource can help you uncover the full burden of your patients’ ulcerative colitis (UC) and align on care goals through early and effective dialogue


For your patients
EFFECTIVE DIALOGUE PATIENT QUESTIONNAIRE
This questionnaire was designed to help patients discuss their UC symptoms and overall well-being with their doctor



References
1. Rubin DT, et al. Inflamm Bowel Dis. 2017;23:494–501.
2. Dubinsky MC, et al. Inflamm Bowel Dis. 2021;27:1747–1755.
3. Larussa T, et al. J Clin Med. 2020;9:2416–2430.
4. Bonsack O, et al. United European Gastroenterol J. 2023;11:361–370.
5. Peyrin-Biroulet L, et al. Dig Liver Dis. 2016;48:601–607.
6. Rubin DT, et al. Inflamm Bowel Dis. 2021;27:1096–1106.
7. Rubin DT, et al. Inflamm Bowel Dis. 2021;27:1942–1953.
8. Murray A, et al. Cochrane Database Syst Rev. 2020;8:CD000544.
9. Loftus EV, et al. Inflamm Bowel Dis. 2014;20:1361–1367.
10. Selinger CP, et al. Aliment Pharmacol Ther. 2017;46:964–973.
11. Esposti LD, et al. Dig Liver Dis. 2023. doi:10.1016/j.dld.2023.04.022.
12. Danese S, et al. Dig Dis. 2019;37:266–283.
13. Denesh D, et al. Expert Rev Gastroenterol Hepatol. 2021;15:1091–1096.
14. Data on file. Pfizer Inc.







